The morphology of skin is comprised of two primary layers of viable tissue that covers nearly the entire surface of the body [1,2]. These layers include the epidermis and dermis interspersed by a basement membrane, all of which reside on a subcutaneous fat layer or hypodermis. Residing in the skin are numerous structural appendages, including the hair follicle, eccrine, and sebaceous glands as well as capillary networks (Fig. 2.1).
The epidermis is the upper (or outermost) layer of the skin and comprises a cellular continuum from the underlying viable cell layers up through to the stratum corneum at the surface. This layer can be further subdivided into four layers: the basal, spinous, granular, and cornified layers (Fig. 2.2). Each cellular layer in the epidermis represents various stages along a process in which basal epidermal keratinocytes undergo a continuous cycle of proliferation, differentiation, and apoptosis moving upward from the basal layer to finally yield corneocytes that make up the stratum corneum. Basal keratinocytes reside at the lower portion of the epidermis supported on the basement membrane that separates the epidermis from the dermis. These mitotically active cells undergo a proliferative cycle to generate daughter cells that are physically dislocated upward into the spinous and granular layers and undergo the process of differentiation into corneocytes. During this process, the cells are attached to each other through desmosome connections via cadherins and
Opening of sweat duct
![]() Sweat duct
Sweat duct
Epidermis
Rete peg
Sebaceous gland
Danish
Dermal nerve fibre
Eccrine sweat duct
Hair follicle
![]() Eccrine sweat gland
Eccrine sweat gland
Muscle
Subcutaneous fat
Figure 2.1 General schematic of skin ‘s architecture.
intracellular keratin proteins become complexed with filaggrin, a large molecular weight protein that is posttranslationally processed (for a general review, see [3]). On passing through the spinous and granular layers, the cells undergo morphological changes that render them flatter in structure as they lose their cellular viability, undergo alternate keratin expression profiles, and transform into cellular remnants. A younger-aged epidermis turns over on average in 28-30 days, and this can rise to 40+ days in older-aged skin. Structurally, the resulting corneocytes remain connected to each other via integrins concentrated in surface desmosomes [4] and are interspersed with lipid bilayer lamellar structures, the latter of which also help provide part of the water barrier properties of skin. The layers of corneocytes in the stratum corneum averages 18-25 and the resulting barrier that is formed provides up to 98% of the water retention ability of the skin. The filaggrin present in cor – neocytes can be proteolytically degraded into small peptide fragments and ultimately into individual amino acids, depending on the relative water state of the upper layers of the epidermis. These amino acids along with urea and lactic acid in the stratum corneum are referred to as the skin’s natural moisturizing factor (NMF). As external humidity changes impact the skin’s water content, the keratin-filaggrin complexes in the corneocytes serve as a repository to generate more NMF via proteolysis to help counterbalance any trans-epidermal water loss. In contrast, exposure of skin to excessive humidity can be deleterious as well, leading to swelling of the stratum corneum and disruption of the lamellar structure bodies.
Other types of cells present in the epidermis include antigen presenting Langerhans, Merkel, and melanocytes. Langerhans cells are macrophages that serve as a primary defense to help prevent infection as well as block aberrant cellular growth as in the case of transformed tumor cells. These cells, along with macrophages in the dermis, are the main reason for the skin to be considered an immunologically related organ, because they function as the initial response when the skin comes into contact with a foreign substance. Merkel cells are essentially modified keratinocytes that are connected via desmosomes to surrounding keratinocytes and also serve the main role of mechanosensory detection via connections to nerve endings.
The melanocytes are specialized dendritic-like cells interspersed amongst basal kerati – nocytes and serve the primary function of producing melanin that is distributed to surrounding keratinocytes. Each melanocyte is in contact with upward of 30 keratinocytes via dendritic processes [5]. Melanin itself is comprised of eumelanin and pheomelanin, two pigmentary components that generate the diversity of coloration observed amongst the global population [6]. The melanins are complex polymers derived from tyrosine, which is converted to DOPA and dopaquinone by tyrosinase, a critical enzyme that is one of the regulatory points for melanogenesis [7]. At the molecular level, the chemistry of melano – genesis is a multistep process that involves a series of oxidative and complexation reactions, including complexation of dopaquinone with cysteine (derived from glutathione), which leads to the production of various forms of pheomelanin and is responsible for yellow or red pigment colors [8]. Pheomelanin is the primary pigment observed in red hair and light-skinned individuals. Alternatively, dopaquinone is converted into dopachrome, which can take two pathways to eumelanin production. Eumelanin is the primary pigment observed in darker-skinned individuals.
The general pigmentation of skin occurs via the active transport of melanin granules called melanosomes to neighboring keratinocytes via the melanocyte’s dendritic processes [9] (Fig. 2.2). Melanosomes are lysosome-like structures whose characteristics
|
Dendrite* |
|
Melanocyte with melano*ome* |
|
Keratlnocyte with melanin granule* over the nuclein |
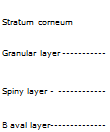 |
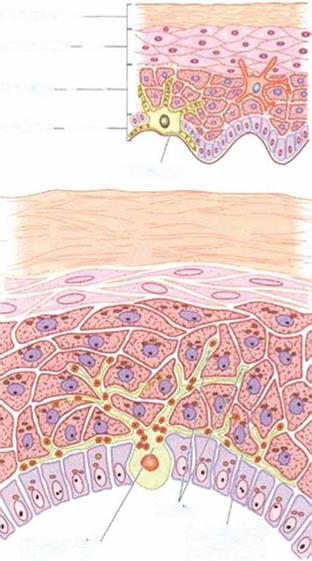 Figure 2.2 The primary layers present in the epidermis and melanin distribution from melanocytes.
Figure 2.2 The primary layers present in the epidermis and melanin distribution from melanocytes.
differ depending on the type of melanin produced. Pheomelanosomes are primitive spherical structures whereas eumelanosomes are oval structures and express three times more tyrosinase than pheomelanosomes. The regulation of melanin production is very complex and involves upward of 80 genes [10,11]. The synthetic process has been found to be regulated by various extracellular signaling components that trigger a signal transduction cascade via melanocortin receptors [12,13]. While the baseline state of melanin in each individual’s skin is dictated by genetic composition, external triggers such as UV irradiation and other forms of stress can lead to significant alterations in net synthesis of the melanins [14].
Underlying the epidermal layer is the basement membrane, a complex cutaneous network comprised of varying collagens, including types IV, VII, and XVII and anchoring fibrils. Published work examining the basement membrane zone (BMZ) has shown that complex hemidesmosome attachments present in the BMZ are critical for maintaining a stable integration between the epidermis and dermis, which is evident in some genetic disorders that leads to blistering of the skin [15]. These hemidesmosomes extend from the basal keratinocytes into the basement membrane. On the dermal side, anchoring fibrils allow for anchorage into the papillary region of the dermis.
The BMZ interface resides on the surface of the dermis, the thickest portion of the skin that makes up 90% of the total skin thickness, and is comprised primarily of various extracellular matrix (ECM) components, which render the skin’s resilience and elasticity. The dermis can be divided into two layers, the papillary and reticular layers. The papillary layer resides immediately under the epidermis and helps provide some of the support to the basement membrane interface as well as extensions into the epidermis that are called rete ridges. These in turn help to maintain the skin’s integrity via a better physical interface between the epidermis and dermis at a macro level. In contrast to the epidermis, the papillary layer is relatively sparse in total cellular content, yet contains mesenchymal-derived dermal fibroblasts. These cells serve the primary function of synthesizing ECM components, which include types I and III collagen, elastin, glycosaminoglycans (GAGs), and fibronectin, of which type I and III collagen make up greater than 85% of the total dermal ECM protein content. Collagen synthesis involves various posttranslational modification steps, including proteolytic removal of N – and C-terminal peptide fragments, arrangement into 3- and 4-triple helix complexes that finally assemble into regularly arranged fibrillar structures.
This blend of the collagen fibrillar network with the other ECM components provides the skin’s strength, elastic, and turgor properties. The ECM content of the papillary layer is relatively densely packed in irregular distributions. Dermal fibroblasts help regulate the overall content, and thereby structural integrity, of the dermis by regulating the resupply of new collagen and the turnover and removal of older or damaged collagen. This occurs via a balance of new collagen synthesis and altered expression patterns of matrix metallopro – teases (MMPs) and tissue inhibitor of matrix metalloproteases (TIMPs). The ability to turnover damaged collagen and repair with newly synthesized collagen is particularly relevant during photodamage, wound healing, and responses to other environmental insults. The reticular layer is sparser in cell content and is comprised of loosely held coarse fibers of collagen and other ECM components such as elastin. It serves as a main structural component to the skin because of its overall thickness and as an anchoring connective tissue for such appendages as sweat glands and hair follicles. Finally, the capillary vasculature that helps supply nutrients and waste removal from the skin resides in the dermis. Thus, when there is an injury that leads to blood loss, there is clear damage that extends through the epidermis into the dermis.
